Dataset of Pulse Waves for Thousands of Virtual Subjects, aged 25-75 years old
The full database can be downloaded from here.
Algorithms used to create the database and for subsequent pulse wave analysis can be found here.
Using Nektar1D, we created a database of 4,374 virtual subjects aged 25-75 years old (in ten year increments), each with distinctive arterial pulse waveforms.
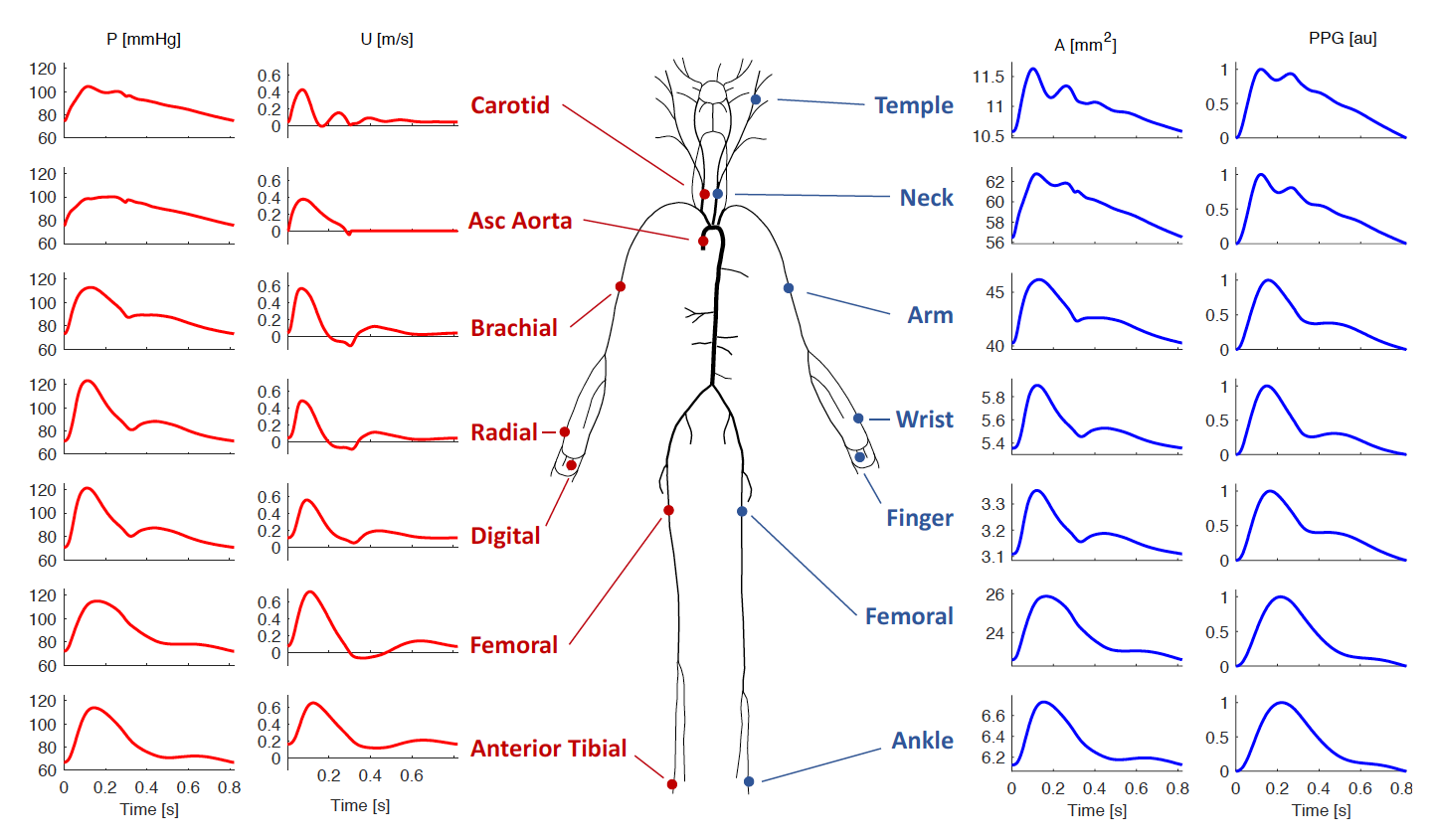
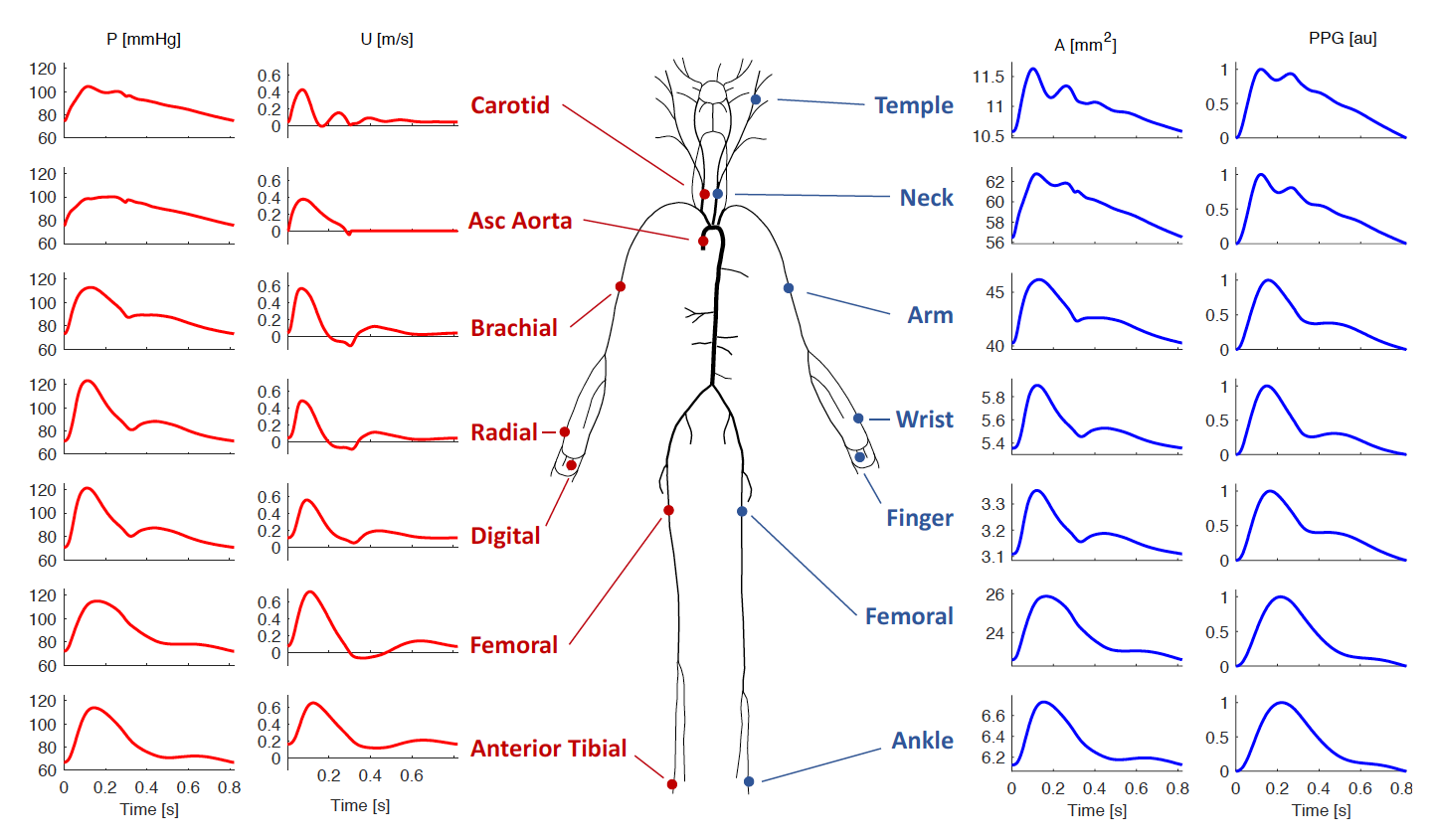
For each subject, arterial blood pressure (P), flow rate (Q), flow velocity (U), luminal area (A), and photoplethysmogram (PPG) pulse waves are available at a range of measurement sites (see figure below), together with the parameters of the simulation (e.g. vessel geometries, cardiac output, arterial stiffness).
This database was designed to be representative of a sample of healthy adults.
 The database was verified by comparing the simulated pulse waves and derived indexes with corresponding in vivo data. Good agreement was observed, with well-reproduced age-related changes in haemodynamic parameters and pulse wave morphology.
The dataset allows for extensive in silico analyses of the performance of pulse wave analysis algorithms, and investigations into the mechanisms of haemodynamics. Its utility for the development and pre-clinical design and assessment of pulse wave analysis techniques was demonstrated with three case studies:
(i) an investigation into the determinants of pulse pressure amplification
(the ratio of brachial to aortic pulse pressure),
which highlighted two main mechanisms responsible
for changes in pulse pressure amplification with age;
(ii) an evaluation of methods for assessing aortic stiffness
(an important marker of cardiovascular health)
from the finger PPG pulse wave,
with key findings to inform the design of future clinical assessments of these algorithms;
and (iii) an evaluation of algorithms for estimating cardiac output from arterial blood pressure waveforms,
with implications for future clinical evaluations of algorithms.
The database was verified by comparing the simulated pulse waves and derived indexes with corresponding in vivo data. Good agreement was observed, with well-reproduced age-related changes in haemodynamic parameters and pulse wave morphology.
The dataset allows for extensive in silico analyses of the performance of pulse wave analysis algorithms, and investigations into the mechanisms of haemodynamics. Its utility for the development and pre-clinical design and assessment of pulse wave analysis techniques was demonstrated with three case studies:
(i) an investigation into the determinants of pulse pressure amplification
(the ratio of brachial to aortic pulse pressure),
which highlighted two main mechanisms responsible
for changes in pulse pressure amplification with age;
(ii) an evaluation of methods for assessing aortic stiffness
(an important marker of cardiovascular health)
from the finger PPG pulse wave,
with key findings to inform the design of future clinical assessments of these algorithms;
and (iii) an evaluation of algorithms for estimating cardiac output from arterial blood pressure waveforms,
with implications for future clinical evaluations of algorithms.
Modeling arterial pulse waves in healthy aging: a database for in silico evaluation of hemodynamics and pulse wave indexes.
American Journal of Physiology: Heart and Circulatory Physiology,
317:H1062-85, 2019

The arterial pulse wave (PW) is a rich source of information on cardiovascular (CV) health. It is widely measured by both consumer and clinical devices. However, the physical determinants of the PW are not yet fully understood, and the development of PW analysis algorithms is limited by a lack of PW data sets containing reference CV measurements. Our aim was to create a database of PWs simulated by a computer to span a range of CV conditions, representative of a sample of healthy adults. The typical CV properties of 25–75 yr olds were identified through a literature review. These were used as inputs to a computational model to simulate PWs for subjects of each age decade. Pressure, flow velocity, luminal area, and photoplethysmographic PWs were simulated at common measurement sites, and PW indexes were extracted. The database, containing PWs from 4,374 virtual subjects, was verified by comparing the simulated PWs and derived indexes with corresponding in vivo data. Good agreement was observed, with well-reproduced age-related changes in hemodynamic parameters and PW morphology. The utility of the database was demonstrated through case studies providing novel hemodynamic insights, in silico assessment of PW algorithms, and pilot data to inform the design of clinical PW algorithm assessments. In conclusion, the publicly available PW database is a valuable resource for understanding CV determinants of PWs and for the development and preclinical assessment of PW analysis algorithms. It is particularly useful because the exact CV properties that generated each PW are known.


