Datasets of Aortic Pressure and Flow Waves for Thousands of Virtual Subjects
Both datasets can be downloaded from here.
In addition, algorithms used to create the datasets and for subsequent pulse wave analysis can be found here.
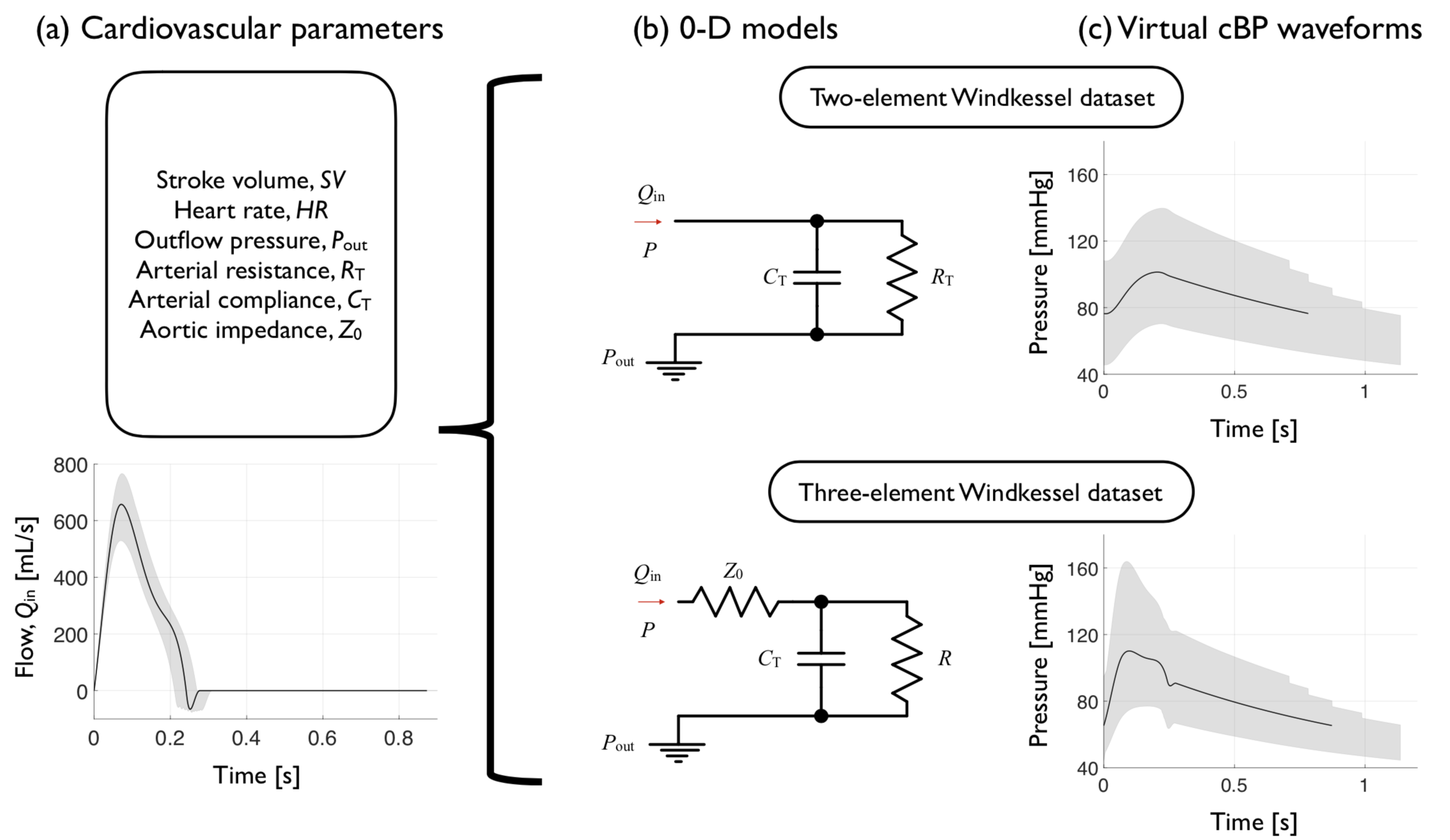
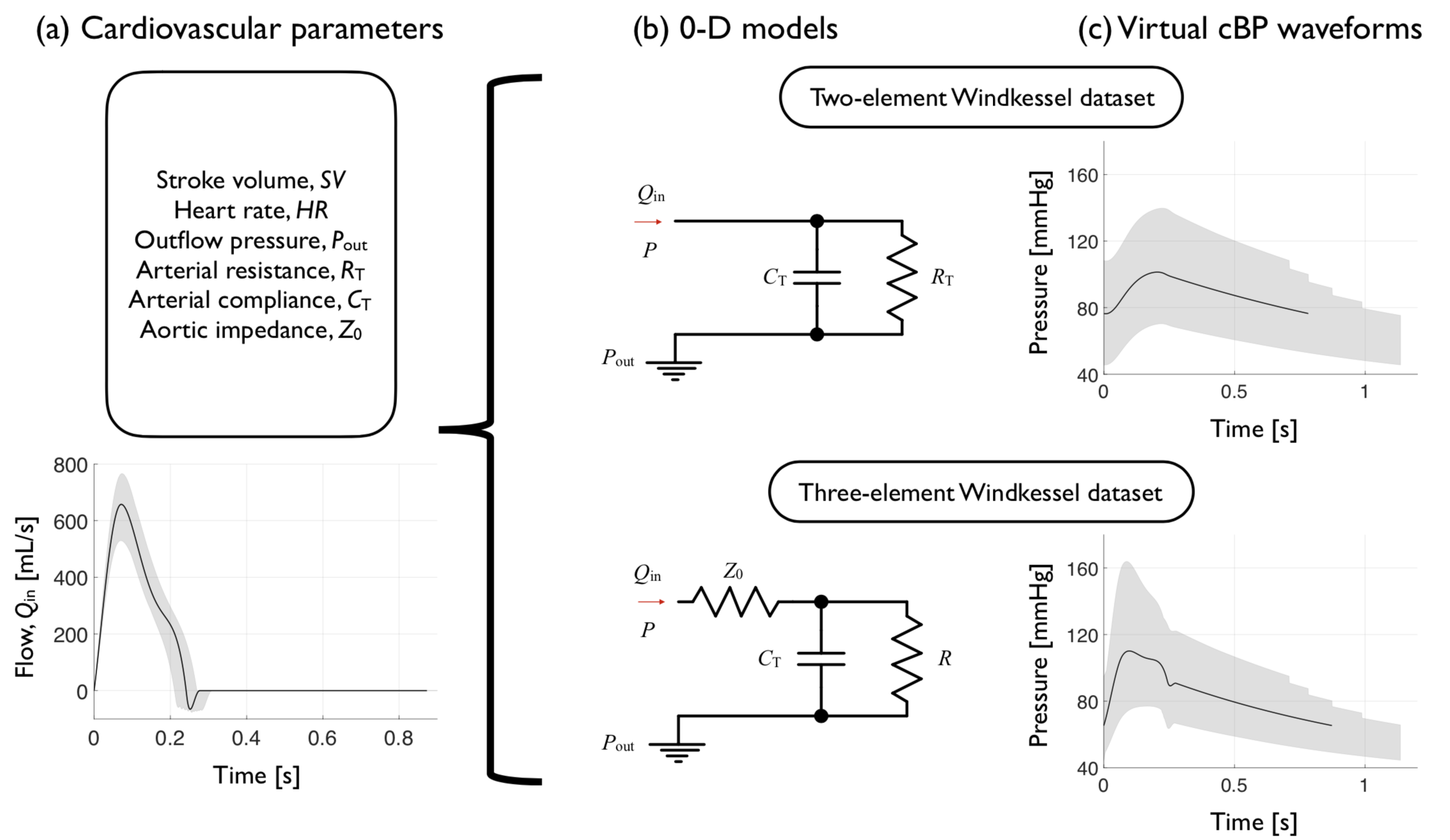
Two datasets containing aortic blood pressure and flow waves for 3,125 and 15,625 virtual subjects were simulated using the two- and three- element Windkessel models, respectively. Each virtual subject’s aortic pressure wave was simulated using an aortic flow wave generated by the AorticFlowWave script (based on prescribed values of heart rate and stroke volume) in combination with prescribed values of arterial resistance and compliance, aortic characteristic impedance, and outflow pressure. These cardiovascular parameters were selected to create two datasets of aortic pressure and flow waves representative of a sample of healthy adults. To do so, 1) mean (m) and standard deviation (SD) values of each parameter in healthy adults were identified from the literature; 2) five values for each parameter were calculated as m, m ± 0.5*SD, and m ± SD; and 3) a virtual subject was created using each of the 3,125 or 15,625 combinations of cardiovascular parameters as input to the two- or three- element Windkessel models, respectively. Further details are given in here.
 The dataset with 15,625 virtual subjects was used to assess several methods for estimating cardiovascular parameters from blood pressure and flow data, as detailed in here.
The dataset with 15,625 virtual subjects was used to assess several methods for estimating cardiovascular parameters from blood pressure and flow data, as detailed in here.
Estimating central blood pressure from aortic flow: development and assessment of algorithms.
American Journal of Physiology: Heart and Circulatory Physiology,
320:H494-510, 2021

Central blood pressure (cBP) is a highly prognostic cardiovascular (CV) risk factor whose accurate, invasive assessment is costly and carries risks to patients. We developed and assessed novel algorithms for estimating cBP from noninvasive aortic hemodynamic data and a peripheral blood pressure measurement. These algorithms were created using three blood flow models: the two- and three-element Windkessel (0-D) models and a one-dimensional (1-D) model of the thoracic aorta. We tested new and existing methods for estimating CV parameters (left ventricular ejection time, outflow BP, arterial resistance and compliance, pulse wave velocity, and characteristic impedance) required for the cBP algorithms, using virtual (simu- lated) subjects (n = 19,646) for which reference CV parameters were known exactly. We then tested the cBP algorithms using virtual subjects (n = 4,064), for which reference cBP were available free of measurement error, and clinical datasets containing invasive (n = 10) and noninvasive (n = 171) reference cBP waves across a wide range of CV conditions. The 1-D algorithm outperformed the 0-D algorithms when the aortic vascular geometry was available, achieving central systolic blood pressure (cSBP) errors 2.1 ± 9.7 mmHg and root-mean-square errors (RMSEs) 6.4 ± 2.8 mmHg against invasive refer- ence cBP waves (n = 10). When the aortic geometry was unavailable, the three-element 0-D algorithm achieved cSBP errors 6.0±4.7mmHg and RMSEs 5.9±2.4mmHg against noninvasive reference cBP waves (n = 171), outperforming the two-element 0-D algorithm. All CV parameters were estimated with mean percentage errors 8.2%, except for the aortic characteristic impedance ( 13.4%), which affected the three-element 0-D algorithm’s performance. The freely available algo- rithms developed in this work enable fast and accurate calculation of the cBP wave and CV parameters in datasets containing noninvasive ultrasound or magnetic resonance imaging data.


