Estimating Central Blood Pressure from Non-Invasive Data
Central blood pressure (cBP) is the blood pressure measured at the ascending aorta next to the heart and therefore the load that the heart has to overcome when pumping. cBP has a higher prognostic value than peripheral blood pressure measured in the arm. However, cBP can only be measured directly with catheterisation, which is costly and carries risks to patients due to its invasive nature. Noninvasive estimation of cBP together with cardiac imaging has the potential to improve cardiovascular function assessment.
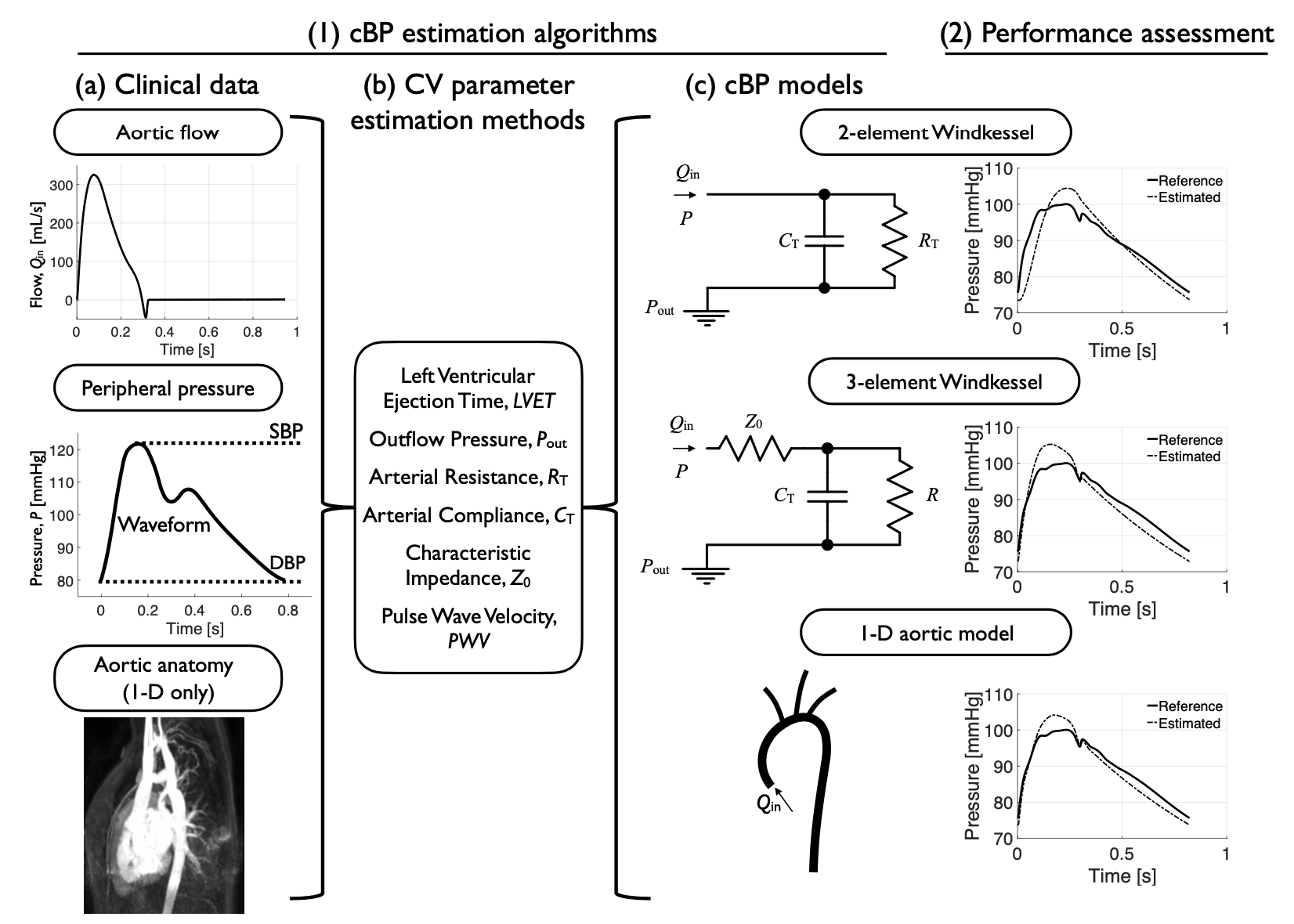
 We have produced algorithms to estimate and analyse the cBP waveform from data that can be acquired non-invasively. Using algorithms based on haemodynamic principles and phenomenon occurring in the aorta itself, we have shown that the cBP waveform can be entirely reconstructed from aortic flow, aortic stiffness, and space-invariant components of blood pressure. More specifically:
We have produced algorithms to estimate and analyse the cBP waveform from data that can be acquired non-invasively. Using algorithms based on haemodynamic principles and phenomenon occurring in the aorta itself, we have shown that the cBP waveform can be entirely reconstructed from aortic flow, aortic stiffness, and space-invariant components of blood pressure. More specifically:
 We have produced algorithms to estimate and analyse the cBP waveform from data that can be acquired non-invasively. Using algorithms based on haemodynamic principles and phenomenon occurring in the aorta itself, we have shown that the cBP waveform can be entirely reconstructed from aortic flow, aortic stiffness, and space-invariant components of blood pressure. More specifically:
We have produced algorithms to estimate and analyse the cBP waveform from data that can be acquired non-invasively. Using algorithms based on haemodynamic principles and phenomenon occurring in the aorta itself, we have shown that the cBP waveform can be entirely reconstructed from aortic flow, aortic stiffness, and space-invariant components of blood pressure. More specifically:
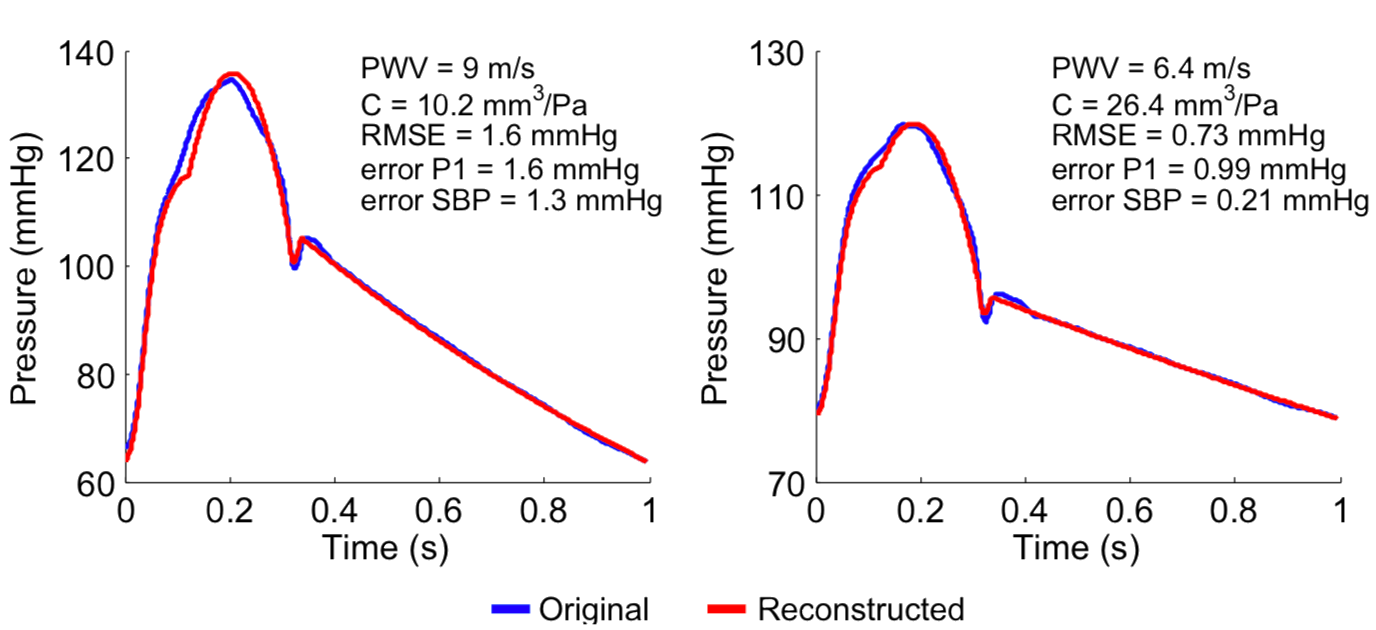
- The cBP wave can be estimated from the aortic flow velocity wave, aortic pulse wave velocity (aPWV), and peripheral pressure components (diastolic decay, diastolic and mean blood pressures) (Am J Physiol, 2015);
- Early cBP systolic components at the time of peak myocardial wall stress (a major indicator of cardiac performance often coinciding with the first systolic shoulder, P1) can be accurately estimated from aPWV and aortic flow (Am J Physiol, 2015);
- Aortic flow velocity may be an important determinant of cardiovascular risk since it links important determinants of cardiovascular risks: the pulsatile cBP components and aPWV (Am J Physiol, 2015);
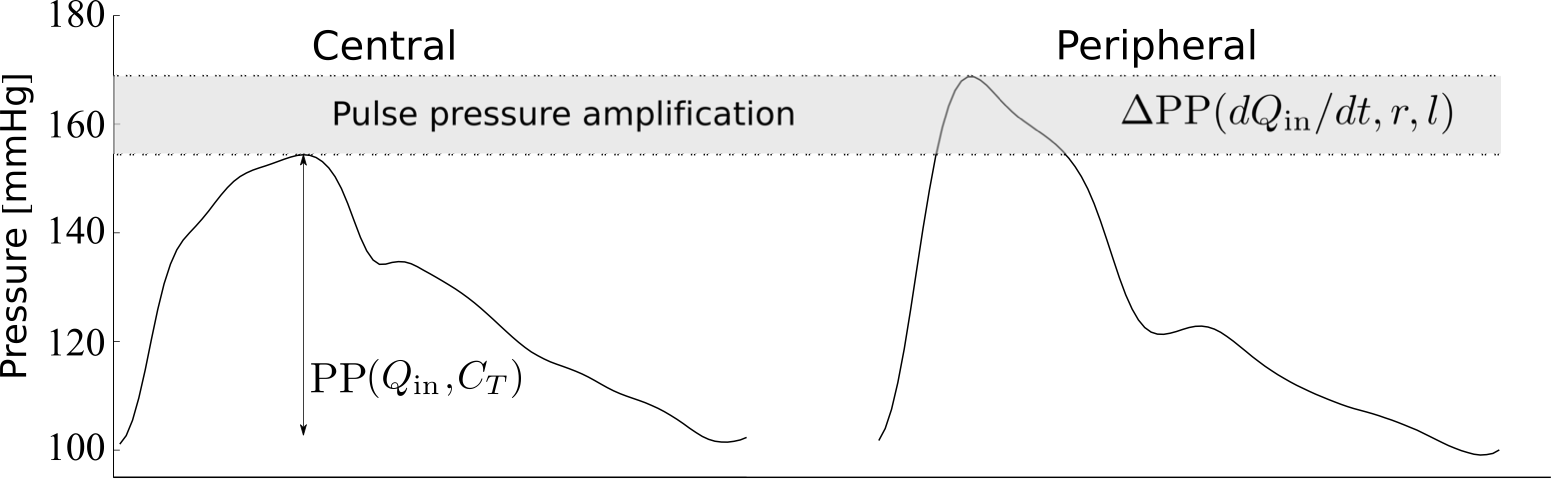
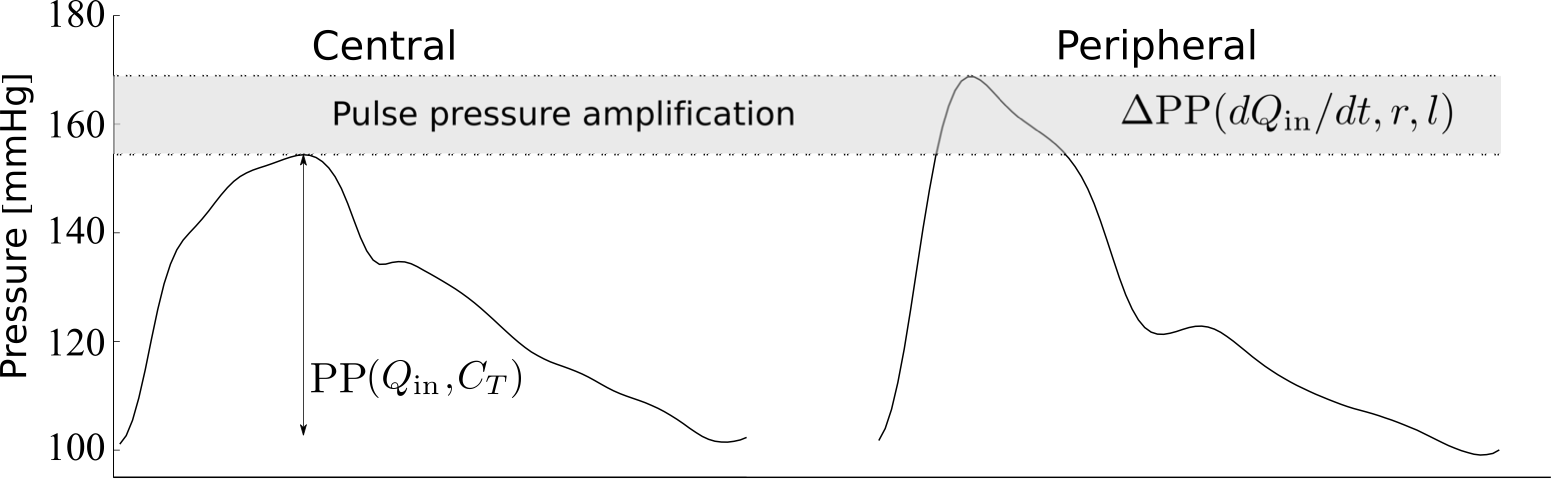
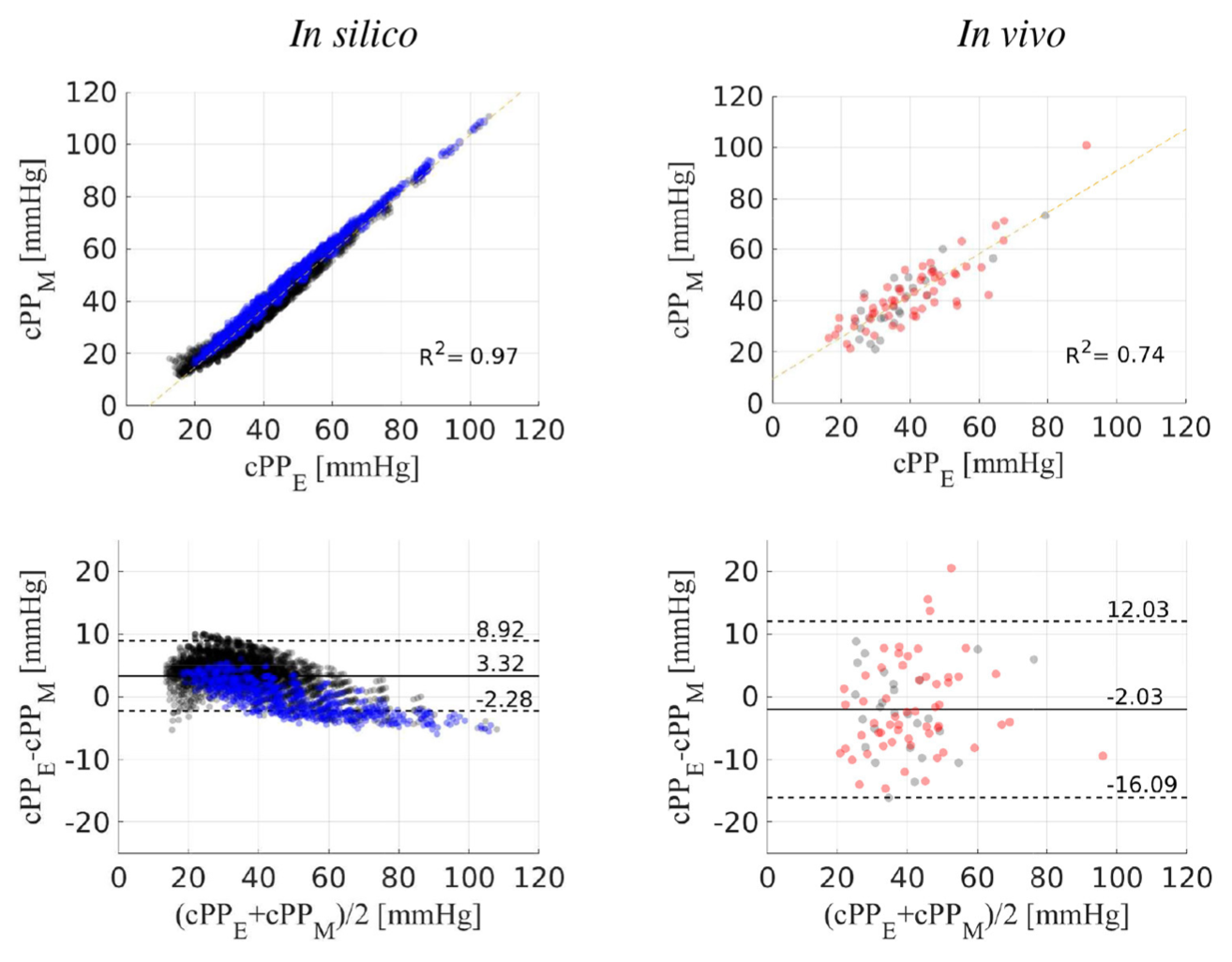
- Central pulse pressure (i.e. the amplitude of the cBP wave which increases with hypertension) can be estimated from non-invasive measurements of aortic flow and peripheral pulse pressure, based on a comprehensive understanding of the main cardiovascular properties that determine pressure amplification along the aortic-brachial arterial path (Frontiers Physiol, 2021);
- Algorithms using computational blood flow modelling (1-D and 0-D models) can be employed to estimate the cBP wave from aortic flow, thoracic aorta properties, and peripheral pressure components (Am J Physiol, 2021). These algorithms are freely available from here;
- 1-D model-based algorithms can outperform 0-D model-based algorithms at estimating cBP wave morphology when the aortic vascular geometry is available (Am J Physiol, 2021).
- In vivo data (including intra-aortic pressure waveforms measured in patients undergoing catheterisation) and in silico data (measured in thousands of virtual subjects), which have allowed us to test our algorithms;
- Robust methods for estimating cardiovascular parameters (left ventricular ejection time, outflow vascular blood pressure, total arterial resistance and compliance, aortic pulse wave velocity, and characteristic impedance) from noninvasive haemodynamic data measured in the thoracic aorta and a peripheral blood measurement (Am J Physiol, 2021) (see here for arterial stiffness quantification). These methods are freely available from here;
- A one-dimensional model of blood flow in the thoracic aorta verified by comparison against in vivo and three-dimensional model data (J Royal Soc Interface, 2016);
- A software tool (developed in collaboration with Philips Healthcare) to extract the arterial geometry and blood inflow profiles from MRI images (Proc Comput Sci, 2016);
- Analytical solutions for the blood pressure and flow waveforms (Frontiers Physiol, 2021; Ann Biomed Eng, 2016);
- Algorithms for reducing the topological complexity of the arterial network (and hence the number of parameters to be estimated), while sufficiently capturing relevant cBP values such as peak blood pressure (J R Soc Interface, 2018; Am J Physiol, 2015).